Understanding the Differences Between Endometriosis and PCOS
Understanding the Differences Between Endometriosis and PCOS
Navigating the realm of reproductive health can be confounding, especially when conditions like Endometriosis and Polycystic Ovarian Syndrome (PCOS) get bundled into one bewildering conversation. Despite affecting millions of individuals in their reproductive years, these conditions differ significantly in their nature, symptoms, and treatment approaches.
To untangle the confusion, it’s crucial to unravel the similarities, dissect the distinctions, and shed light on these two separate health concerns.
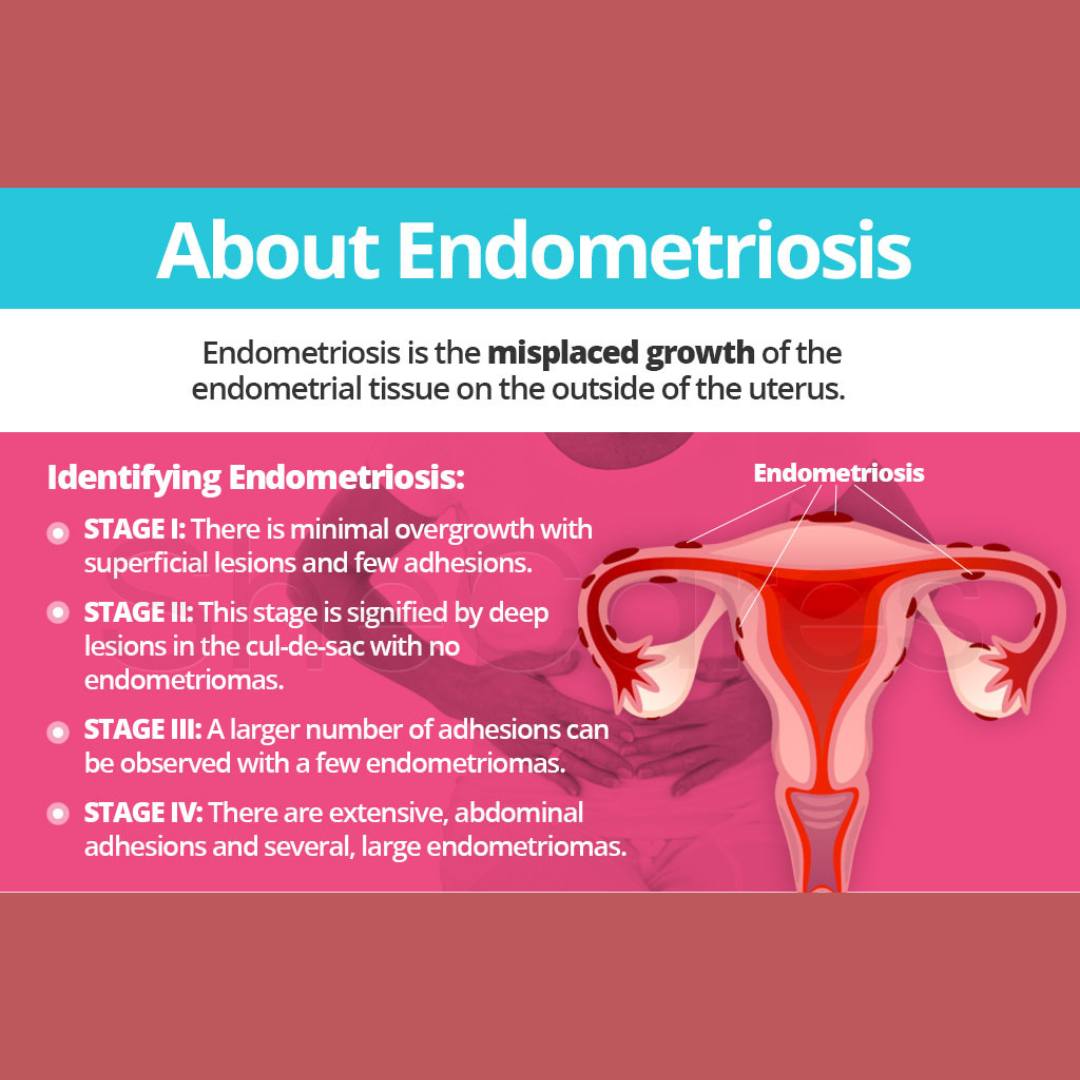
What is Endometriosis?
Endometriosis, a condition notorious for its excruciating pain, impacts about 190 million females globally. Studies suggest it affects around 10–15% women, highlighting the substantial number embroiled in the battle against endo.
This chronic and progressive medical condition involves tissue resembling the uterine lining (endometrium) migrating to unconventional territories. It establishes itself outside the uterus, spreading across the ovaries, fallopian tubes, pelvic tissue, and occasionally extending beyond the pelvic region.
This rebellious relocation of tissue isn’t merely an inconvenience; it brings about severe pain and life-altering consequences. Its impact extends beyond menstrual periods, causing discomfort during or after sex and even distress during urination.
Moreover, along with the agonizing pain, an array of unwelcome symptoms emerge: abdominal bloating, nausea, fatigue, depression, anxiety, chronic pelvic pain, heavy bleeding during or between periods, and challenges in conceiving.
The exact cause remains elusive to doctors. However, certain factors might elevate the risk of developing endometriosis, including retrograde menstruation, aberrant cell behavior outside the uterus, estrogen influence, immune system anomalies, family history, prolonged and heavy menstrual cycles, early onset of menstruation, low body weight, alcohol consumption, and later pregnancies.
Managing endometriosis poses challenges, given the absence of a cure. Some individuals resort to pain relievers or hormonal medications like birth control pills, IUDs such as Mirena®, or patches. Surgery can offer relief but doesn't promise a permanent fix.
Understanding PCOS:
In contrast to endometriosis, Polycystic Ovarian Syndrome (PCOS) revolves around hormonal irregularities. It affects up to 20% of women during their reproductive years and ranks among the leading causes of infertility. An estimated 80% of individuals experiencing fertility challenges due to ovulation issues may have PCOS.
The condition arises from elevated levels of male hormones produced by the ovaries, impacting the menstrual cycle and various bodily functions. Its origins remain enigmatic, but it's believed to have ties with increased insulin levels.
Genetics or lifestyle factors might contribute to PCOS. Its symptoms span irregular menstrual cycles, mood swings, sleep disturbances, persistent acne, obesity, and excessive hair growth on the face and body.
Despite the name "polycystic ovary syndrome," the cysts associated with PCOS aren't actual cysts but rather misunderstood egg follicles. Diagnosis necessitates consultations with a doctor, along with blood tests and ultrasounds, as it's not a condition that can be self-diagnosed.
Early diagnosis proves pivotal in managing symptoms and averting long-term complications. It warrants proactive measures because PCOS escalates the risk of Type 2 or gestational diabetes, sexual health issues, sleep apnoea, or heart disorders.
If you’re diagnosed with PCOS, your doctor may recommend medication. You may also be advised to undertake some PCOS self-care, like eating a specific diet and exercising more, to help deal with the physical and emotional symptoms that go along with the condition. Dealing with PCOS can be a bit of a rollercoaster ride, but it’s manageable with the right tools and support.
PCOS vs endometriosis: they’re both painful, but they’re not the same thing. While endo and PCOS are similar in that they are both a pain in the uterus (and other bits), they are fundamentally different and should be diagnosed by a medical professional. By getting up to speed on the facts, you can make informed decisions about your best care plan.
Eco Period products can provide support for both disorders during times of heavy or irregular bleeding, thanks to their varying levels of absorbency. Our period undies are tested for maximum comfort and performance, making difficult periods easier to manage.
Yoni Steaming can also help remedy the following: cramps and pain, clots, fibroids, cysts, endometriosis, infections, dryness, absent cycles, adhesions, polycystic ovarian syndrome, infertility, postpartum, and preparation for birth.
According to various case studies, vaginal steaming appears to improve symptoms in over 90% of all gynecological problems and shows tremendous potential as an alternative to invasive medical procedures. Most gynecologists will tell you not to try it, with the premise that the vagina is self-cleaning and exposing the perineum and surrounding area to heat will upset the “delicate” balance and flora of the vagina. Medical practitioners are misinformed about the practice because it is beyond their scope of training and expertise, as this is a cultural wellness practice.
The Peristeam Hydrotherapist Institute in California is collecting testimonials of people who use vaginal steam to assess whether or not they find the practice beneficial. Participants are asked to rate their health concerns prior to and after vaginal steaming to compare if there is a decline in negative symptoms. Please check the link to see the testimonials.
"I have a 29 day cycle for the first time in my life. I don’t have flash flood bleeding and debilitating cramps. My period only lasts 4 days. These things are totally new and complete game changers for my quality of life. I don’t lose days at work anymore."
If you feel drawn to try our steam herb blends, please reach out and chat to us about the best blend for you. Typically we want to know if you have any active infections, if your cycle length is currently regular and if it is a short cycle under 28 days from the start of each period.